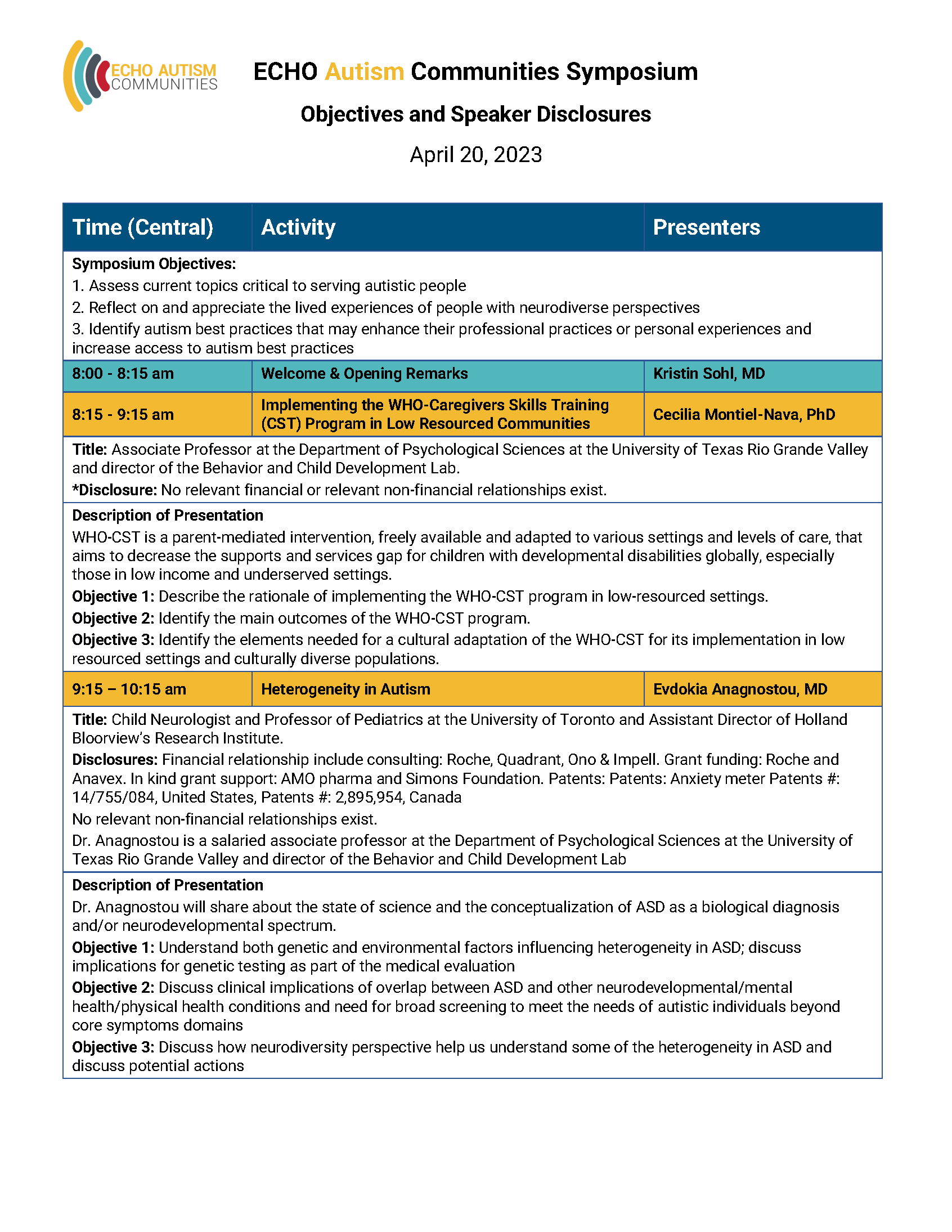
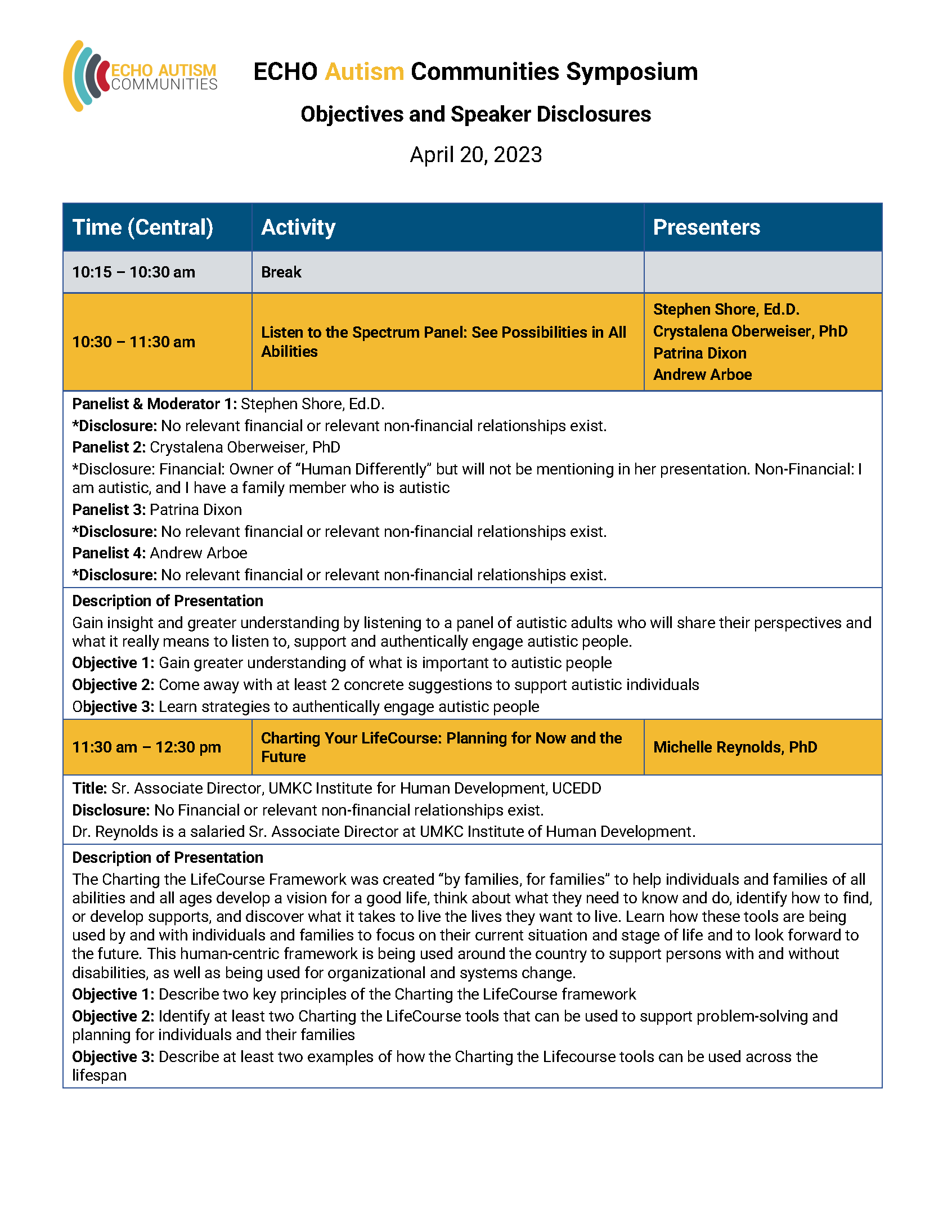
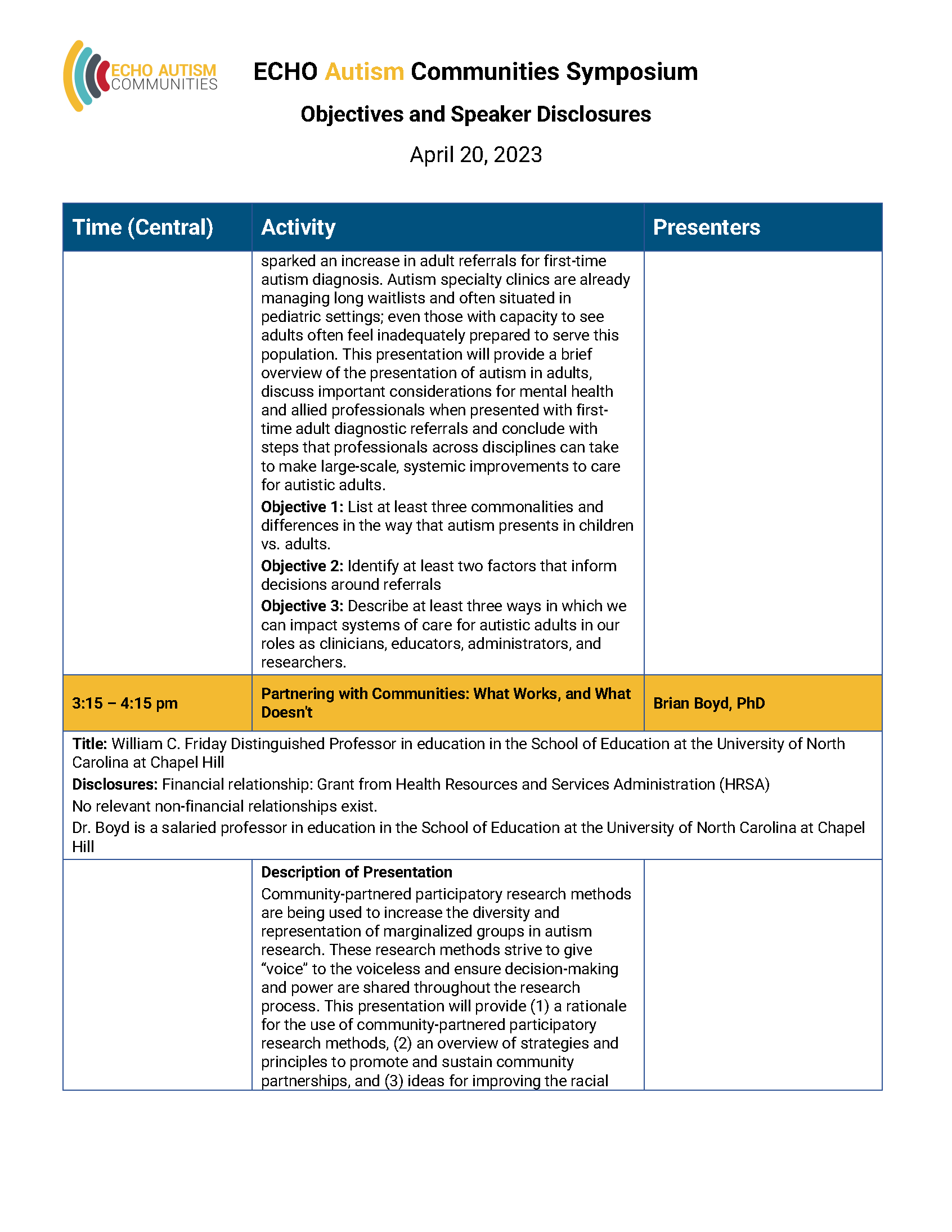
September 2020
Building Equity and Supporting BIPOC Families of Individuals with Autism
Families often face long wait times and challenges to get their children not only an autism diagnosis, but services and care throughout an individual’s whole life. But what about when race is involved?
Research has shown us that Black, Indigenous, and People of Color (BIPOC) often have implicit biases, lack of understanding, and even systemic racism to overcome in the healthcare system. This creates an additional layer of stress to an already stressful journey of raising a child with autism and navigating complex systems throughout their course of life. To provide the respect, services, and supports that families deserve, autism professionals must do the work to build authentic and trusting relationships with our people with autism and their families.
In our latest webinar, Building Equity and Supporting Black and Brown Families of Individuals with Autism, our expert guest panel will cover a myriad of topics related to race and healthcare, including understanding historical context, how to address your own implicit bias, how to practice having conversations about race, and the benefit of learning from others experiences.
To get you started in the conversation, check out these clips from the overall conversation. You can find the full webinar on our Youtube channel by clicking here.
Why Should We Discuss Marginalized Communities?
Historically, black and brown families have had a harder time accessing autism services and receiving a diagnosis than white families. In a study just published in the September issue of Pediatrics, researchers found that there was, on average, a three year delay between the parent’s first concern for developmental delay and an ASD diagnosis with black children.
“Moreover, nearly half of parents reported visiting multiple providers before receiving an ASD diagnosis, and 31.3% stated lack of available professionals contributed to this delay,” the study explained.
Dr. Jennifer Sykes, a licensed psychologist at the University of Missouri Columbia Thompson Center, and guest expert on the panel, emphasizes the importance of separating things out by race.
“There’s such an intersectional piece that comes into ‘yes you have an autism diagnosis,’ but also you are a person of color,” Jennifer DeLaporte, research specialist and special education teacher, discusses. “People experience the world differently. Your experiences dictate how you move and interact with the world. If we don’t start to acknowledge those differences, so that we can build on those and give validation to those differences, then we continue to perpetuate the problem of not seeing the full story.”
Developing authentic relationships between patient and practitioner is how BIPOC families are going to be served better.
Recognizing Implicit Bias
Our guest panel dives into the idea of “implicit bias,” the idea that people are coming to the table with a foundation of prejudices or stereotypes without intention, or necessarily, realization.
According to our experts, empirical evidence has demonstrated that white medical care clinicals have implicit racial biases that persist independently of and in contrast to their conscious racial attitudes, but that will still affect their decision making and behavior during their interactions with BIPOC patients.
“You don’t have to be an overt racist using racial slurs and harassing your neighbor of color, you can carry these biases in you, and honestly, we all do. There’s been a lot of research that talks about how we tend to view black children as older than they are by three or four years, so that’s a pretty big deal,” explains Dr. Jennifer Sykes, licensed psychologist at the University of Missouri.
All of this, in turn, affects how black and brown families are treated in the health care system. Their levels of mistrust in white providers, on top of the lengthy path to access services, creates barriers to these families getting the right care, at the right time, at the right place.
Doing the Work
Throughout the webinar, our panel discusses what “doing the work” really looks like, and how it can make us all better health care providers. From learning safety signals, to becoming anti-racist, to understanding that your patients are having different experiences all goes into fully understanding how to best serve marginalized communities. We must do the work to become a trusted source of medical advice for ALL families and eliminate discrimination in the healthcare system.
To watch the whole webinar, click here.